A Way To Combat Fallen Arches
Overview

Feet usually have an arch on the inside portion of the foot. A flat foot is a foot that has lost or never developed this arch. It is often associated with the lower part of the legs being angled outwards. Most flat feet are flexible. This type rarely causes problems and usually do not require treatment. Rigid flat feet can cause problems and are best treated.
Causes
Family history, experts say fallen arches can run in families. Weak arch, the arch of the foot may be there when no weight is placed on it, for example, when the person is sitting. But as soon as they stand up the foot flattens (falls) onto the ground. Injury, arthritis, tibialis posterior (ruptured tendon), pregnancy, nervous system or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida. Tarsal Coalition, the bones of the foot fuse together in an unusual way, resulting in stiff and flat feet. Most commonly diagnosed during childhood. Diabetes. Age and wear and tear, years of using your feet to walk, run, and jump eventually may take its toll. One of the eventual consequences could be fallen arches. The posterior tibial tendon may become weakened after long-term wear a tear. The postario tibial tendon is the main support structure of the arch of our feet. The tendon can become inflamed (tendinitis) after overuse - sometimes it can even become torn. Once the tendon is damaged, the arch shape of the foot may flatten.
Symptoms
Having flat feet can be painless and is actually normal in some people. But others with flat feet experience pain in the heel or arch area, difficulty standing on tiptoe, or have swelling along the inside of the ankle. They may also experience pain after standing for long periods of time or playing sports. Some back problems can also be attributed to flat feet.
Diagnosis
Your doctor examines your feet to determine two things, whether you have flat feet and the cause or causes. An exam may include the following steps, Checking your health history for evidence of illnesses or injuries that could be linked to flat feet or fallen arches, Looking at the soles of your shoes for unusual wear patterns, Observing the feet and legs as you stand and do simple movements, such as raising up on your toes, Testing the strength of muscles and tendons, including other tendons in the feet and legs, such as the Achilles tendon or the posterior tibial tendon, Taking X-rays or an MRI of your feet.
deelsonheels
Non Surgical Treatment
If your condition is bothersome, try elevating your feet and using ice on the arches to reduce swelling. Your podiatrist can recommend several orthotic aids and inserts to strengthen the tendons of your foot. He can also demonstrate stretching exercises or refer you to physical therapy to get those tendons back into shape. If the symptoms of fallen arches are painful and troubling, he may recommend a steroid injection to relieve inflammation and pain. And in some instances, he may determine that surgery is necessary.
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.
Prevention
Flatfeet in children are often an inherited family trait, but it may be possible to prevent the condition in some cases. Recent research has shown that there are several social or cultural factors that can cause flatfeet. These factors include the following, obesity, overweight, unnecessary orthopedic treatments, wearing rigid shoes at a young age, In 1992, a study in India of 2300 children aged 4-13 demonstrated a significant difference in the rate of flatfeet among those who wore shoes regularly and those who did not. In this study, wearing inflexible, closed-toe shoes in early childhood was shown to have a negative effect on the normal development of arches. Children who were allowed to go barefoot or who wore light sandals and slippers had a much lower rate of flatfeet. In 1999, a study in Spain of 1181 children aged 4-13 revealed that the use of orthopedic shoes for treatment of flatfeet in children not only failed to correct the problem, but actually worsened the condition by preventing the normal flexing and arch development of bare or lightly protected feet. Finally, in 2006, a study of 835 children aged 3-6 showed significant differences in the rate of flatfeet based on weight, with normal-weight children having lower rates of flatfeet than children who were overweight or obese. Among adults, flatfeet due to injury, disease, or normal aging are not preventable. However, when flatfeet are related to lifestyle factors, such as physical activities, shoe selection, and weight gain, careful attention to these factors may prevent the development of flatfeet.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.

Feet usually have an arch on the inside portion of the foot. A flat foot is a foot that has lost or never developed this arch. It is often associated with the lower part of the legs being angled outwards. Most flat feet are flexible. This type rarely causes problems and usually do not require treatment. Rigid flat feet can cause problems and are best treated.
Causes
Family history, experts say fallen arches can run in families. Weak arch, the arch of the foot may be there when no weight is placed on it, for example, when the person is sitting. But as soon as they stand up the foot flattens (falls) onto the ground. Injury, arthritis, tibialis posterior (ruptured tendon), pregnancy, nervous system or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida. Tarsal Coalition, the bones of the foot fuse together in an unusual way, resulting in stiff and flat feet. Most commonly diagnosed during childhood. Diabetes. Age and wear and tear, years of using your feet to walk, run, and jump eventually may take its toll. One of the eventual consequences could be fallen arches. The posterior tibial tendon may become weakened after long-term wear a tear. The postario tibial tendon is the main support structure of the arch of our feet. The tendon can become inflamed (tendinitis) after overuse - sometimes it can even become torn. Once the tendon is damaged, the arch shape of the foot may flatten.
Symptoms
Having flat feet can be painless and is actually normal in some people. But others with flat feet experience pain in the heel or arch area, difficulty standing on tiptoe, or have swelling along the inside of the ankle. They may also experience pain after standing for long periods of time or playing sports. Some back problems can also be attributed to flat feet.
Diagnosis
Your doctor examines your feet to determine two things, whether you have flat feet and the cause or causes. An exam may include the following steps, Checking your health history for evidence of illnesses or injuries that could be linked to flat feet or fallen arches, Looking at the soles of your shoes for unusual wear patterns, Observing the feet and legs as you stand and do simple movements, such as raising up on your toes, Testing the strength of muscles and tendons, including other tendons in the feet and legs, such as the Achilles tendon or the posterior tibial tendon, Taking X-rays or an MRI of your feet.
deelsonheels
Non Surgical Treatment
If your condition is bothersome, try elevating your feet and using ice on the arches to reduce swelling. Your podiatrist can recommend several orthotic aids and inserts to strengthen the tendons of your foot. He can also demonstrate stretching exercises or refer you to physical therapy to get those tendons back into shape. If the symptoms of fallen arches are painful and troubling, he may recommend a steroid injection to relieve inflammation and pain. And in some instances, he may determine that surgery is necessary.
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.
Prevention
Flatfeet in children are often an inherited family trait, but it may be possible to prevent the condition in some cases. Recent research has shown that there are several social or cultural factors that can cause flatfeet. These factors include the following, obesity, overweight, unnecessary orthopedic treatments, wearing rigid shoes at a young age, In 1992, a study in India of 2300 children aged 4-13 demonstrated a significant difference in the rate of flatfeet among those who wore shoes regularly and those who did not. In this study, wearing inflexible, closed-toe shoes in early childhood was shown to have a negative effect on the normal development of arches. Children who were allowed to go barefoot or who wore light sandals and slippers had a much lower rate of flatfeet. In 1999, a study in Spain of 1181 children aged 4-13 revealed that the use of orthopedic shoes for treatment of flatfeet in children not only failed to correct the problem, but actually worsened the condition by preventing the normal flexing and arch development of bare or lightly protected feet. Finally, in 2006, a study of 835 children aged 3-6 showed significant differences in the rate of flatfeet based on weight, with normal-weight children having lower rates of flatfeet than children who were overweight or obese. Among adults, flatfeet due to injury, disease, or normal aging are not preventable. However, when flatfeet are related to lifestyle factors, such as physical activities, shoe selection, and weight gain, careful attention to these factors may prevent the development of flatfeet.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Do You Understand Heel Aches?
Overview

The most common cause of heel pain is plantar fasciitis. Many patients with plantar fasciitis have a heel spur on the front and bottom of their heel, but heel spurs do not cause pain. The common name is "heel spur" because it's easier to pronounce than "plantar fasciitis" and doctors are able to point to the spur on an x-ray. Causes of heel pain include inadequate flexibility in the calf muscles, lack of arch support, being overweight, suddenly increasing activity, and spending too much time on the feet. Arch support was rated the best treatment in our first survey of 1,800 visitors to heelspurs.com. The Plantar Fasciitis Orthotic is getting the best customer reviews and it is the most popular product. It is new for 2011. Returning customers may be seeking the Pinnacle Orthotic. The primary difference is that the PF Orthotic should be used only for current cases of plantar fasciitis or heel spurs and the Pinnacle is best for general use once the condition has subsided. Survery respondents also benefited from: rest, ice, tape, and night splints.
Causes
Heel pain can have many causes. If your heel hurts, see your primary care doctor or orthopaedic foot and ankle specialist right away to determine why and get treatment. Tell him or her exactly where you have pain and how long you've had it. Your doctor will examine your heel, looking and feeling for signs of tenderness and swelling. You may be asked to walk, stand on one foot or do other physical tests that help your doctor pinpoint the cause of your sore heel. Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel.
Symptoms
Usually when a patient comes in they?ll explain that they have severe pain in the heel. It?s usually worse during the first step in the morning when they get out of bed. Many people say if they walk for a period of time, it gets a little bit better. But if they sit down and get back up, the pain will come back and it?s one of those intermittent come and go types of pain. Heel pain patients will say it feels like a toothache in the heel area or even into the arch area. A lot of times it will get better with rest and then it will just come right back. So it?s one of those nuisance type things that just never goes away. The following are common signs of heel pain and plantar fasciitis. Pain that is worse first thing in the morning. Pain that develops after heavy activity or exercise. Pain that occurs when standing up after sitting for a long period of time. Severe, toothache type of pain in the bottom of the heel.
Diagnosis
In most cases, your GP or a podiatrist (a specialist in foot problems and foot care) should be able to diagnose the cause of your heel pain by asking about your symptoms and medical history, examining your heel and foot.
Non Surgical Treatment
To properly treat heel pain, you must absorb shock, provide cushioning and elevate the heel to transfer pressure. This can be accomplished with a heel cup, visco heel cradle, or an orthotic designed with materials that will absorb shock and shear forces. When the condition is pronation related (usually plantar fasciitis), an orthotic with medial posting and good arch support will control the pronation and prevent the inflammation of the plantar fascia. Footwear selection is also an important criteria when treating heel pain. Shoes with a firm heel counter, good arch support, and appropriate heel height are the ideal choice. If the problem persists, consult your foot doctor.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
foot pain heel
Prevention

You can reduce the risk of heel pain in many ways, including. Wear shoes that fit you properly with a firm fastening, such as laces. Choose shoes with shock-absorbent soles and supportive heels. Repair or throw out any shoes that have worn heels. Always warm up and cool down when exercising or playing sport, include plenty of slow, sustained stretches. If necessary, your podiatrist will show you how to tape or strap your feet to help support the muscles and ligaments. Shoe inserts (orthoses) professionally fitted by your podiatrist can help support your feet in the long term.

The most common cause of heel pain is plantar fasciitis. Many patients with plantar fasciitis have a heel spur on the front and bottom of their heel, but heel spurs do not cause pain. The common name is "heel spur" because it's easier to pronounce than "plantar fasciitis" and doctors are able to point to the spur on an x-ray. Causes of heel pain include inadequate flexibility in the calf muscles, lack of arch support, being overweight, suddenly increasing activity, and spending too much time on the feet. Arch support was rated the best treatment in our first survey of 1,800 visitors to heelspurs.com. The Plantar Fasciitis Orthotic is getting the best customer reviews and it is the most popular product. It is new for 2011. Returning customers may be seeking the Pinnacle Orthotic. The primary difference is that the PF Orthotic should be used only for current cases of plantar fasciitis or heel spurs and the Pinnacle is best for general use once the condition has subsided. Survery respondents also benefited from: rest, ice, tape, and night splints.
Causes
Heel pain can have many causes. If your heel hurts, see your primary care doctor or orthopaedic foot and ankle specialist right away to determine why and get treatment. Tell him or her exactly where you have pain and how long you've had it. Your doctor will examine your heel, looking and feeling for signs of tenderness and swelling. You may be asked to walk, stand on one foot or do other physical tests that help your doctor pinpoint the cause of your sore heel. Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel.
Symptoms
Usually when a patient comes in they?ll explain that they have severe pain in the heel. It?s usually worse during the first step in the morning when they get out of bed. Many people say if they walk for a period of time, it gets a little bit better. But if they sit down and get back up, the pain will come back and it?s one of those intermittent come and go types of pain. Heel pain patients will say it feels like a toothache in the heel area or even into the arch area. A lot of times it will get better with rest and then it will just come right back. So it?s one of those nuisance type things that just never goes away. The following are common signs of heel pain and plantar fasciitis. Pain that is worse first thing in the morning. Pain that develops after heavy activity or exercise. Pain that occurs when standing up after sitting for a long period of time. Severe, toothache type of pain in the bottom of the heel.
Diagnosis
In most cases, your GP or a podiatrist (a specialist in foot problems and foot care) should be able to diagnose the cause of your heel pain by asking about your symptoms and medical history, examining your heel and foot.
Non Surgical Treatment
To properly treat heel pain, you must absorb shock, provide cushioning and elevate the heel to transfer pressure. This can be accomplished with a heel cup, visco heel cradle, or an orthotic designed with materials that will absorb shock and shear forces. When the condition is pronation related (usually plantar fasciitis), an orthotic with medial posting and good arch support will control the pronation and prevent the inflammation of the plantar fascia. Footwear selection is also an important criteria when treating heel pain. Shoes with a firm heel counter, good arch support, and appropriate heel height are the ideal choice. If the problem persists, consult your foot doctor.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
foot pain heel
Prevention

You can reduce the risk of heel pain in many ways, including. Wear shoes that fit you properly with a firm fastening, such as laces. Choose shoes with shock-absorbent soles and supportive heels. Repair or throw out any shoes that have worn heels. Always warm up and cool down when exercising or playing sport, include plenty of slow, sustained stretches. If necessary, your podiatrist will show you how to tape or strap your feet to help support the muscles and ligaments. Shoe inserts (orthoses) professionally fitted by your podiatrist can help support your feet in the long term.
How To Calculate For Leg Length Discrepancy
Overview
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
Causes
There are many causes of leg length discrepancy. Some include, A broken leg bone may lead to a leg length discrepancy if it heals in a shortened position. This is more likely if the bone was broken in many pieces. It also is more likely if skin and muscle tissue around the bone were severely injured and exposed, as in an open fracture. Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. A break in a child's bone through the growth center near the end of the bone may cause slower growth, resulting in a shorter leg. Bone infections that occur in children while they are growing may cause a significant leg length discrepancy. This is especially true if the infection happens in infancy. Inflammation of joints during growth may cause unequal leg length. One example is juvenile arthritis. Bone diseases may cause leg length discrepancy, as well. Examples are, Neurofibromatosis, Multiple hereditary exostoses, Ollier disease. Other causes include inflammation (arthritis) and neurologic conditions. Sometimes the cause of leg length discrepancy is unknown, particularly in cases involving underdevelopment of the inner or outer side of the leg, or partial overgrowth of one side of the body. These conditions are usually present at birth, but the leg length difference may be too small to be detected. As the child grows, the leg length discrepancy increases and becomes more noticeable. In underdevelopment, one of the two bones between the knee and the ankle is abnormally short. There also may be related foot or knee problems. Hemihypertrophy (one side too big) or hemiatrophy (one side too small) are rare leg length discrepancy conditions. In these conditions, the arm and leg on one side of the body are either longer or shorter than the arm and leg on the other side of the body. There may also be a difference between the two sides of the face. Sometimes no cause can be found. This is known as an "idiopathic" difference.
Symptoms
The most common symptom of all forms of LLD is chronic backache. In structural LLD the sufferer may also experience arthritis within the knee and hip are, flank pain, plantar fasciitis and metatarsalgia all on the side that is longer. Functional LLD sufferers will see similar conditions on the shorter side.
Diagnosis
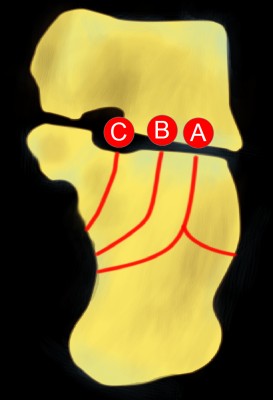
There are several orthopedic tests that are used, but they are rudimentary and have some degree of error. Even using a tape measure with specific anatomic landmarks has its errors. Most leg length differences can be seen with a well trained eye, but I always recommend what is called a scanagram, or a x-ray bone length study (see picture above). This test will give a precise measurement in millimeters of the length difference.
Non Surgical Treatment
The non-surgical intervention is mainly usedfor the functional and environmental types of leg length discrepancies. It is also applied to the mild category of limb length inequality. Non-surgical intervention consists of stretching the muscles of the lower extremity. This is individually different, whereby the M. Tensor Fascia latae, the adductors, the hamstring muscles, M. piriformis and M. Iliopsoas are stretched. In this non-surgical intervention belongs also the use of shoe lifts. These shoe lifts consists of either a shoe insert (up to 10-20mm of correction), or building up the sole of the shoe on the shorter leg (up to 30-60mm of correction). This lift therapy should be implemented gradually in small increments. Several studies have examined the treatment of low back pain patients with LLD with shoe lifts. Gofton obtained good results: the patients experienced major or complete pain relief that lasted upon follow-up ranging from 3 to 11 years. Helliwell also observed patients whereby 44% experienced complete pain relief, and 45% had moderate or substantial pain relief. Friberg found that 157 (of 211) patients with LBP, treated with shoe lifts, were symprom-free after a mean follow-up of 18 months.

leg length discrepancy measurement
Surgical Treatment
Bone growth restriction (epiphysiodesis) The objective of this surgical procedure is to slow down growth in the longer leg. During surgery, doctors alter the growth plate of the bone in the longer leg by inserting a small plate or staples. This slows down growth, allowing the shorter leg to catch up over time. Your child may spend a night in the hospital after this procedure or go home the same day. Doctors may place a knee brace on the leg for a few days. It typically takes 2 to 3 months for the leg to heal completely. An alternative approach involves lengthening the shorter bone. We are more likely to recommend this approach if your child is on the short side of the height spectrum.
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.

Causes
There are many causes of leg length discrepancy. Some include, A broken leg bone may lead to a leg length discrepancy if it heals in a shortened position. This is more likely if the bone was broken in many pieces. It also is more likely if skin and muscle tissue around the bone were severely injured and exposed, as in an open fracture. Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. A break in a child's bone through the growth center near the end of the bone may cause slower growth, resulting in a shorter leg. Bone infections that occur in children while they are growing may cause a significant leg length discrepancy. This is especially true if the infection happens in infancy. Inflammation of joints during growth may cause unequal leg length. One example is juvenile arthritis. Bone diseases may cause leg length discrepancy, as well. Examples are, Neurofibromatosis, Multiple hereditary exostoses, Ollier disease. Other causes include inflammation (arthritis) and neurologic conditions. Sometimes the cause of leg length discrepancy is unknown, particularly in cases involving underdevelopment of the inner or outer side of the leg, or partial overgrowth of one side of the body. These conditions are usually present at birth, but the leg length difference may be too small to be detected. As the child grows, the leg length discrepancy increases and becomes more noticeable. In underdevelopment, one of the two bones between the knee and the ankle is abnormally short. There also may be related foot or knee problems. Hemihypertrophy (one side too big) or hemiatrophy (one side too small) are rare leg length discrepancy conditions. In these conditions, the arm and leg on one side of the body are either longer or shorter than the arm and leg on the other side of the body. There may also be a difference between the two sides of the face. Sometimes no cause can be found. This is known as an "idiopathic" difference.
Symptoms
The most common symptom of all forms of LLD is chronic backache. In structural LLD the sufferer may also experience arthritis within the knee and hip are, flank pain, plantar fasciitis and metatarsalgia all on the side that is longer. Functional LLD sufferers will see similar conditions on the shorter side.
Diagnosis
There are several orthopedic tests that are used, but they are rudimentary and have some degree of error. Even using a tape measure with specific anatomic landmarks has its errors. Most leg length differences can be seen with a well trained eye, but I always recommend what is called a scanagram, or a x-ray bone length study (see picture above). This test will give a precise measurement in millimeters of the length difference.
Non Surgical Treatment
The non-surgical intervention is mainly usedfor the functional and environmental types of leg length discrepancies. It is also applied to the mild category of limb length inequality. Non-surgical intervention consists of stretching the muscles of the lower extremity. This is individually different, whereby the M. Tensor Fascia latae, the adductors, the hamstring muscles, M. piriformis and M. Iliopsoas are stretched. In this non-surgical intervention belongs also the use of shoe lifts. These shoe lifts consists of either a shoe insert (up to 10-20mm of correction), or building up the sole of the shoe on the shorter leg (up to 30-60mm of correction). This lift therapy should be implemented gradually in small increments. Several studies have examined the treatment of low back pain patients with LLD with shoe lifts. Gofton obtained good results: the patients experienced major or complete pain relief that lasted upon follow-up ranging from 3 to 11 years. Helliwell also observed patients whereby 44% experienced complete pain relief, and 45% had moderate or substantial pain relief. Friberg found that 157 (of 211) patients with LBP, treated with shoe lifts, were symprom-free after a mean follow-up of 18 months.

leg length discrepancy measurement
Surgical Treatment
Bone growth restriction (epiphysiodesis) The objective of this surgical procedure is to slow down growth in the longer leg. During surgery, doctors alter the growth plate of the bone in the longer leg by inserting a small plate or staples. This slows down growth, allowing the shorter leg to catch up over time. Your child may spend a night in the hospital after this procedure or go home the same day. Doctors may place a knee brace on the leg for a few days. It typically takes 2 to 3 months for the leg to heal completely. An alternative approach involves lengthening the shorter bone. We are more likely to recommend this approach if your child is on the short side of the height spectrum.
Mortons Neuroma Solutions
Overview
 Some sources claim that entrapment of the plantar nerve because of compression between the metatarsal heads, as originally proposed by Morton, is highly unlikely, because the plantar nerve is on the plantar side of the transverse metatarsal ligament and thus does not come in contact with the metatarsal heads. It is more likely that the transverse metatarsal ligament is the cause of the entrapment. Despite the name, the condition was first correctly described by a chiropodist named Durlacher, and although it is labeled a "neuroma", many sources do not consider it a true tumor, but rather a perineural fibroma (fibrous tissue formation around nerve tissue).
Some sources claim that entrapment of the plantar nerve because of compression between the metatarsal heads, as originally proposed by Morton, is highly unlikely, because the plantar nerve is on the plantar side of the transverse metatarsal ligament and thus does not come in contact with the metatarsal heads. It is more likely that the transverse metatarsal ligament is the cause of the entrapment. Despite the name, the condition was first correctly described by a chiropodist named Durlacher, and although it is labeled a "neuroma", many sources do not consider it a true tumor, but rather a perineural fibroma (fibrous tissue formation around nerve tissue).
Causes
The cause of this problem is often due to impingement of the plantar nerve fibres between the metatarsal heads and the intermetatarsal ligament. It is entirely a biomechanical phenomenon. Differential diagnoses include stress fracture, capsulitis, bursitis or ligament injury at the metatarsal-phalangeal joint, a tendon sheath ganglion, foreign-body reaction and nerve-sheath tumour.
Symptoms
The symptoms of Morton?s Neuroma tend to come and go over time. They are typically exacerbated by physical activity or by wearing certain shoes. Morton?s Neuroma symptoms include sharp pain in the ball of the foot, pain radiating to the tips of the toes, burning pain in the second, third, or fourth toes, numbness in the toes, sensation of a lump between the toes.
Diagnosis
The clinical symptoms should quickly lead your doctor to suspect a neuroma. When examined, the doctor may feel a "click" which is known as Mulder's sign. There may be tenderness in the interspace. The metatarsal bones will also be examined both clinically (and often with an xray). Tenderness at one of the metatarsal bones can suggest an overstress reaction (pre-stress fracture or stress fracture) in the bone. An ultrasound scan can confirm the diagnosis and is a less expensive and at this time, at least as sensitive a test as an MRI. An x-ray does not show neuromas, but can be useful to "rule out" other causes of the pain.
Non Surgical Treatment
Treatment strategies for Morton's neuroma range from conservative to surgical management. The conservative approach to treating Morton's neuroma may benefit from the involvement of a physical therapist. The physical therapist can assist the physician in decisions regarding the modification of footwear, which is the first treatment step. Recommend soft-soled shoes with a wide toe box and low heel (eg, an athletic shoe). High-heeled, narrow, nonpadded shoes should not be worn, because they aggravate the condition. The next step in conservative management is to alter alignment of the metatarsal heads. One recommended action is to elevate the metatarsal head medial and adjacent to the neuroma, thereby preventing compression and irritation of the digital nerve. A plantar pad is used most often for elevation. Have the patient insert a felt or gel pad into the shoe to achieve the desired elevation of the above metatarsal head. Other possible physical therapy treatment ideas for patients with Morton's neuroma include cryotherapy, ultrasonography, deep tissue massage, and stretching exercises. Ice is beneficial to decrease the associated inflammation. Phonophoresis also can be used, rather than just ultrasonography, to further decrease pain and inflammation.
Surgical Treatment
The ultimate success of a Morton?s neuroma treated surgically is somewhat unclear. This is likely due to the idea that in most instances a ?Morton?s neuroma? is actually more than just an isolated nerve problem but rather consitutes a metatarsalgia where other structures (such a as the MTP joints) are also problematic, not just the nerve. Therefore, addressing the nerve as well as the other components of a metatarsalgia may offer a better chance of surgical success. However, like many conditions in foot and ankle, it is ideal if this condition can be managed without surgery.
 Some sources claim that entrapment of the plantar nerve because of compression between the metatarsal heads, as originally proposed by Morton, is highly unlikely, because the plantar nerve is on the plantar side of the transverse metatarsal ligament and thus does not come in contact with the metatarsal heads. It is more likely that the transverse metatarsal ligament is the cause of the entrapment. Despite the name, the condition was first correctly described by a chiropodist named Durlacher, and although it is labeled a "neuroma", many sources do not consider it a true tumor, but rather a perineural fibroma (fibrous tissue formation around nerve tissue).
Some sources claim that entrapment of the plantar nerve because of compression between the metatarsal heads, as originally proposed by Morton, is highly unlikely, because the plantar nerve is on the plantar side of the transverse metatarsal ligament and thus does not come in contact with the metatarsal heads. It is more likely that the transverse metatarsal ligament is the cause of the entrapment. Despite the name, the condition was first correctly described by a chiropodist named Durlacher, and although it is labeled a "neuroma", many sources do not consider it a true tumor, but rather a perineural fibroma (fibrous tissue formation around nerve tissue).Causes
The cause of this problem is often due to impingement of the plantar nerve fibres between the metatarsal heads and the intermetatarsal ligament. It is entirely a biomechanical phenomenon. Differential diagnoses include stress fracture, capsulitis, bursitis or ligament injury at the metatarsal-phalangeal joint, a tendon sheath ganglion, foreign-body reaction and nerve-sheath tumour.
Symptoms
The symptoms of Morton?s Neuroma tend to come and go over time. They are typically exacerbated by physical activity or by wearing certain shoes. Morton?s Neuroma symptoms include sharp pain in the ball of the foot, pain radiating to the tips of the toes, burning pain in the second, third, or fourth toes, numbness in the toes, sensation of a lump between the toes.
Diagnosis
The clinical symptoms should quickly lead your doctor to suspect a neuroma. When examined, the doctor may feel a "click" which is known as Mulder's sign. There may be tenderness in the interspace. The metatarsal bones will also be examined both clinically (and often with an xray). Tenderness at one of the metatarsal bones can suggest an overstress reaction (pre-stress fracture or stress fracture) in the bone. An ultrasound scan can confirm the diagnosis and is a less expensive and at this time, at least as sensitive a test as an MRI. An x-ray does not show neuromas, but can be useful to "rule out" other causes of the pain.
Non Surgical Treatment
Treatment strategies for Morton's neuroma range from conservative to surgical management. The conservative approach to treating Morton's neuroma may benefit from the involvement of a physical therapist. The physical therapist can assist the physician in decisions regarding the modification of footwear, which is the first treatment step. Recommend soft-soled shoes with a wide toe box and low heel (eg, an athletic shoe). High-heeled, narrow, nonpadded shoes should not be worn, because they aggravate the condition. The next step in conservative management is to alter alignment of the metatarsal heads. One recommended action is to elevate the metatarsal head medial and adjacent to the neuroma, thereby preventing compression and irritation of the digital nerve. A plantar pad is used most often for elevation. Have the patient insert a felt or gel pad into the shoe to achieve the desired elevation of the above metatarsal head. Other possible physical therapy treatment ideas for patients with Morton's neuroma include cryotherapy, ultrasonography, deep tissue massage, and stretching exercises. Ice is beneficial to decrease the associated inflammation. Phonophoresis also can be used, rather than just ultrasonography, to further decrease pain and inflammation.

Surgical Treatment
The ultimate success of a Morton?s neuroma treated surgically is somewhat unclear. This is likely due to the idea that in most instances a ?Morton?s neuroma? is actually more than just an isolated nerve problem but rather consitutes a metatarsalgia where other structures (such a as the MTP joints) are also problematic, not just the nerve. Therefore, addressing the nerve as well as the other components of a metatarsalgia may offer a better chance of surgical success. However, like many conditions in foot and ankle, it is ideal if this condition can be managed without surgery.
The Solution To Leg Length Discrepancy Are Shoe Lifts
There are not one but two unique variations of leg length discrepancies, congenital and acquired. Congenital implies that you are born with it. One leg is anatomically shorter compared to the other. Through developmental periods of aging, the brain senses the stride pattern and identifies some difference. Your body typically adapts by tilting one shoulder over to the "short" side. A difference of under a quarter inch isn't very excessive, does not need Shoe Lifts to compensate and generally doesn't have a profound effect over a lifetime.

Leg length inequality goes typically undiscovered on a daily basis, however this problem is easily solved, and can reduce a number of cases of back problems.
Treatment for leg length inequality typically consists of Shoe Lifts. These are generally economical, frequently being less than twenty dollars, compared to a custom orthotic of $200 or higher. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Chronic back pain is the most common ailment afflicting men and women today. Around 80 million men and women are affected by back pain at some point in their life. It's a problem which costs companies millions year after year as a result of time lost and output. Fresh and better treatment methods are continually sought after in the hope of lowering economic impact this condition causes.

Men and women from all corners of the world suffer the pain of foot ache as a result of leg length discrepancy. In most of these cases Shoe Lifts might be of immense help. The lifts are capable of eliminating any pain in the feet. Shoe Lifts are recommended by countless specialist orthopaedic orthopedists.
To be able to support the human body in a well-balanced manner, feet have a significant job to play. Despite that, it's often the most neglected zone of the human body. Some people have flat-feet which means there is unequal force placed on the feet. This will cause other body parts such as knees, ankles and backs to be affected too. Shoe Lifts guarantee that proper posture and balance are restored.

Leg length inequality goes typically undiscovered on a daily basis, however this problem is easily solved, and can reduce a number of cases of back problems.
Treatment for leg length inequality typically consists of Shoe Lifts. These are generally economical, frequently being less than twenty dollars, compared to a custom orthotic of $200 or higher. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Chronic back pain is the most common ailment afflicting men and women today. Around 80 million men and women are affected by back pain at some point in their life. It's a problem which costs companies millions year after year as a result of time lost and output. Fresh and better treatment methods are continually sought after in the hope of lowering economic impact this condition causes.

Men and women from all corners of the world suffer the pain of foot ache as a result of leg length discrepancy. In most of these cases Shoe Lifts might be of immense help. The lifts are capable of eliminating any pain in the feet. Shoe Lifts are recommended by countless specialist orthopaedic orthopedists.
To be able to support the human body in a well-balanced manner, feet have a significant job to play. Despite that, it's often the most neglected zone of the human body. Some people have flat-feet which means there is unequal force placed on the feet. This will cause other body parts such as knees, ankles and backs to be affected too. Shoe Lifts guarantee that proper posture and balance are restored.
The Diagnosis Of Inferior Calcaneal Spur
Overview
A common cause of heel pain is the heel spur, a bony growth on the underside of the heel bone. The spur, visible by X-ray, appears as a protrusion that can extend forward as much as half an inch. When there is no indication of bone enlargement, the condition is sometimes referred to as "heel spur syndrome." Heel spurs result from strain on the muscles and ligaments of the foot, by stretching of the long band of tissue that connects the heel and the ball of the foot, and by repeated tearing away of the lining or membrane that covers the heel bone. These conditions may result from biomechanical imbalance, running or jogging, improperly fitted or excessively worn shoes, or obesity.
Causes
A heel spur can develop when there is an abundance of calcium creating a deposit in the calcaneus, or heel bone. Over time, this deposit grows to create an outcropping under the heel that extends into the foot. The result is a protrusion that leads to foot pain when pressure is applied, and in some cases, even during rest.
Symptoms
If your body has created calcium build-ups in an effort to support your plantar fascia ligament, each time you step down with your foot, the heel spur is being driven into the soft, fatty tissue which lines the bottom of your heel. Heel spur sufferers experience stabbing sensations because the hard protrusion is literally being jabbed into the heel pad. If left untreated, Plantar Fasciitis and heel spurs can erode the fatty pad of the heel and cause permanent damage to the foot. Fortunately, most cases can be resolved without medications or surgeries.
Diagnosis
Because the diagnosis of heel spurs can be confused with tarsal tunnel syndrome (as described earlier), most surgeons advocate performing a tarsal tunnel release (or at least a partial tarsal tunnel release) along with the plantar fascia release. This surgery is about 80percent successful in relieving pain in the small group of patients who do not improve with conservative treatments.
Non Surgical Treatment
Rest your foot. Reduce the amount of weight-bearing activities you participate in. Get off of your feet and elevate them. This will allow healing to begin. Apply ice to your foot. Applications of ice packs that provide a comfortable cooling to the heel and arch (not a freezing cold) will help reduce pain, swelling, and inflammation. Apply the ice to the heel and arch (not the toes). Make sure it is comfortable, and leave on your foot for about 20 minutes, 3 times a day. If you have any medical problems such as diabetes, poor circulation, etc., discuss the use of ice with your doctor before applying the ice. Active Wrap allows you to apply comfortable cold therapy to your foot without messy ice cubes. Use while on the ?go.? Do not walk with bare feet. Always protect your heels, arches, and plantar fascia with good supportive shoes. Vionic Orthotic Flip Flops For Men and Women are designed for walking comfort with built in orthotic foot beds that help reduce foot pain from heel spurs. Use in the house or on the beach.
Surgical Treatment
Usually, heel spurs are curable with conservative treatment. If not, heel spurs are curable with surgery, although there is the possibility of them growing back. About 10% of those who continue to see a physician for plantar fascitis have it for more than a year. If there is limited success after approximately one year of conservative treatment, patients are often advised to have surgery.
Does A Inferior Calcaneal Spur Hurt?
Overview
A bone spur (osteophyte) is a bony growth that forms along the edge of normal bone in response to wear and tear, most frequently in the joints. A heel spur is a bone spur of the heel bone, which causes heel pain by rubbing on the achilles tendon or other soft tissues.
Causes
Heel Spur typically occurs in people who have a history of foot pain, and is most often seen in middle-aged men and women. The bony growth itself is not what causes the pain associated with heel spur. The pain is typically caused by inflammation and irritation of the surrounding tissues. Approximately 50% of patients with a heel spur also experience Plantar Fasciitis.

Symptoms
You may or may not experience any symptoms with your heel spurs. It is normally the irritation and inflammation felt in the tissues around your heel spur that cause discomfort. Heel pain is one of the first things you may notice, especially when pushing off the ball of your foot (stretches the plantar fascia). The pain can get worse over time and tends to be stronger in the morning, subsiding throughout the day; although it does return with increased activity. A sharp, poking pain in your heel that feels like you're stepping on a stone can often be felt while standing or walking. You will sometimes be able to feel a bump on the bottom of your heel, and occasionally bruising may appear.
Diagnosis
Your doctor will discuss your medical history and will examine your foot and heel for any deformities and inflammation (swelling, redness, heat, pain). He/she will analyze your flexibility, stability, and gait (the way you walk). Occasionally an x-ray or blood tests (to rule out diseases or infections) may be requested.
Non Surgical Treatment
Diathermy treatment uses an electrical current to produce heat that sedates the inflamed tissues. The ultrasound device sends sound waves into the heel and sets up a massaging action that stimulates blood circulation. Treatment with a whirlpool bath involves placing the foot directly into the jetting stream. Orthopedic molds and appliances, such as orthotics, are designed by foot specialists for use inside the shoe to eliminate irritation to the heel when the patient stands or walks. When those appliances are used, the spur (in effect) floats on air. At the same time, the body's weight is transferred forward from the tender spot.
Surgical Treatment
Surgery to correct for heel spur syndrome is a common procedure which releases plantar fascia partially from its attachment to the calcaneous (heel bone). This part of the surgery is called a plantar fasciotomy due to the fact the fascia is cut. This is most often done through an open procedure as any heel spur or bursa can be removed at the same time. If the spur is not removed during the surgery, it will probably be just as successful, as the large spur is not the true problem. Some physicians use an endoscopic approach (EPF) where a small camera aids the physician during surgery with typically smaller incisions on each side of your foot.